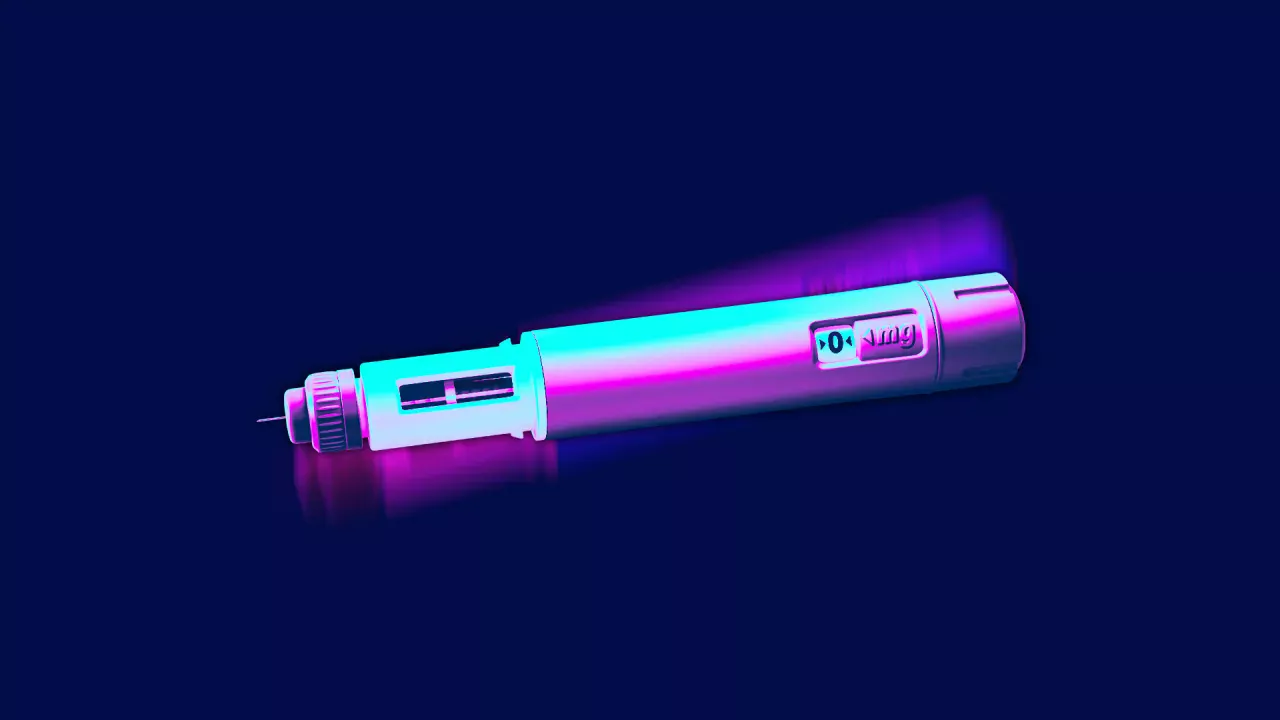
In just a few years, brand-name injectable drugs such as Ozempic, Wegovy, Mounjaro, and Zepbound have rocketed to fame as billion-dollar annual sellers for weight loss as well as to control blood sugar levels and reduce the risk of heart disease.
But the price of these injections is steep: They cost about $800-$1,000 per month, and if used for weight loss alone, they are not covered by most insurance policies. Both drugs mimic the naturally occurring hormone GLP-1 to help regulate blood sugar and reduce cravings. They can be taken only with a prescription.
The Food and Drug Administration (FDA) announced an official shortage of the active ingredients in these drugs in 2022, but on Oct. 2, 2024, the agency announced that the shortage has been resolved for the medicine tirzepatide, the active ingredient in Mounjaro and Zepbound.
Despite the soaring demand and limited supply of these drugs, there are no generic versions available. This is because the patents for semaglutide—the active ingredient in Ozempic and Wegovy, which is still in shortage—and tirzepatide don’t expire until 2033 and 2036, respectively.
As a result, nonbrand alternatives that can be purchased with or without a prescription are flooding the market. Yet these products come with real risks to consumers.
I am a pharmacist who studies weaknesses in federal oversight of prescription and over-the-counter drugs and dietary supplements in the U.S. My research group recently had investigated loopholes that are allowing alternative weight-loss products to enter the market.
High demand is driving GLP-1 wannabes
The dietary supplement market has sought to cash in on the GLP-1 demand with pills, teas, extracts, and all manner of other products that claim to produce similar effects as the brand names at a much lower price.
Products containing the herb berberine offer only a few pounds of weight loss, while many dietary supplement weight-loss products contain stimulants, such as sibutramine, and laxatives, such as phenolphthalein, which increase the risk of heart attacks, strokes and cancer.
The role of compounding pharmacies
Unlike the dietary supplements that are masquerading as GLP-1 weight loss products, compounding pharmacies can create custom versions of products that contain the same active ingredients as the real thing for patients who cannot use either brand or generic products for some reason.
These pharmacies can also produce alternative versions of brand-name drugs when official drug shortages exist.
Since the demand for GLP-1 medications has far outpaced the supply, compounding pharmacies are legally producing a variety of different semaglutide and tirzepatide products.
These products may come in versions that differ from the brand-name companies, such as vials of powder that must be dissolved in liquid or as tablets or nasal sprays.
Just like the brand-name drugs, you must have a valid prescription to receive them. The prices range from $250-$400 a month—still a steep price for many consumers.
Compounding pharmacies must adhere to the FDA’s sterility and quality production methods, but these rules are not as rigorous for compounding pharmacies as those for commercial manufacturers of generic drugs.
In addition, the products compounding pharmacies create do not have to be tested in humans for safety or effectiveness like brand-name products do.
Proper dosing can also be challenging with compounded forms of the drugs.
Companies that work the system
For people who cannot afford a compounding-pharmacy product, or cannot get a valid prescription for semaglutide or tirzepatide, opportunistic companies are stepping in to fill the void. These include “peptide companies,” manufacturers that create non-FDA approved knockoff versions of the drugs.
From November 2023 to March 2024, my team carried out a study to assess which of these peptide companies are selling semaglutide or tirzepatide products. We scoured the internet looking for these peptide companies and collected information about what they were selling and their sales practices.
We found that peptide sellers use a loophole to sell these drugs. On their websites, the companies state that their drugs are for “research purposes only” or “not for human consumption,” but they do nothing to verify that the buyers are researchers or that the product is going to a research facility.
By reading the comments sections of the company websites and the targeted ads on social media, it becomes clear that both buyers and sellers understand the charade. Unlike compounding pharmacies, these peptide sellers do not provide the supplies you need to dissolve and inject the drug, provide no instructions, and will usually not answer questions.
Peptide sellers, since they allegedly are not selling to consumers, do not require a valid prescription and will sell consumers whatever quantity of drug they wish to purchase. Even if a person has an eating disorder such as anorexia nervosa, the companies will happily sell them a semaglutide or tirzepatide product without a prescription. The average prices of these peptide products range from $181-$203 per month.
Skirting regulations
Peptide sellers do not have to adhere to the rules or regulations that drug manufacturers or compounding pharmacies do. Many companies state that their products are 99% pure, but an independent investigation of three companies’ products from August 2023 to March 2024 found that the purity of the products were far less than promised.
One product contained endotoxin—a toxic substance produced by bacteria—suggesting that it was contaminated with microbes. In addition, the products’ promised dosages were off by 29% to 39%. Poor purity can cause patients to experience fever, chills, nausea, skin irritation, infections, and low blood pressure.
In this study, some companies never even shipped the drug, telling the buyers they needed to pay an additional fee to have the product clear customs.
If a consumer is harmed by a poor-quality product, it would be difficult to sue the seller, since the products specifically say they are “not for human consumption.” Ultimately, consumers are being led to spend money on products that may never arrive, could cause an infection, might not have the correct dose, and contain no instructions on how to safely use or store the product.
Will prices for brand-name products come down?
To combat these alternative sellers, pharmaceutical company Eli Lilly began offering an alternative version of its brand-name Zepbound product for weight loss in September 2024.
Instead of its traditional injection pen products that cost more than $1,000 for a month’s supply, this product comes in vials that patients draw up and inject themselves. For patients who take 5 milligrams of Zepbound each week, the vial products would cost them $549 a month if patients buy it through the company’s online pharmacy and can show that they do not have insurance coverage for the drug.
After a grilling on Capitol Hill in September 2024, pharmaceutical company Novo Nordisk came under intense pressure to offer patients without prescription coverage a lower-priced product for its brand-name Wegovy as well.
In the next few years, additional brand-name GLP-1 agonist drugs will likely make it to market. As of October 2024, a handful of these products are in late-phase clinical trials, with active ingredients such as retatrutide, survodutide, and ecnoglutide, and more than 18 other drug candidates are in earlier stages of development.
When new pharmaceutical companies enter this market, they will have to offer patients lower prices than Eli Lilly and Novo Nordisk in order to gain market share. This is the most likely medium-term solution to drive down the costs of GLP-1 drugs and eliminate the drug shortages in the marketplace.
C. Michael White is a distinguished professor of pharmacy practice at the University of Connecticut.
This article is republished from The Conversation under a Creative Commons license. Read the original article.